The importance of early treatment for DMD
Once muscle function is lost, it cannot be restored for children with DMD.1,2
Without adequate care and treatment, patients with DMD typically lose walking ability by their early teens, require ventilation support in their late teens and eventually experience premature death due to heart and lung failure.3
Administering DMD treatment as early as possible is therefore crucial to increase the potential for slowing down disease progression and to help preserve muscle function for as long as possible.1,4,5
Expert insights
Want to understand the benefits of a multidisciplinary care team and why it is important to have an individualised DMD care plan?
Learn more from our DMD experts.
The DMD multidisciplinary care team*
DMD care can be complex. It requires multiple interventions, including neuromuscular, respiratory, cardiac, orthopaedic, endocrine and rehabilitative. These will evolve over the course of the disease.4
As such, international standards of care for DMD recommend a coordinated, multidisciplinary approach to care.4,6,7
By assembling a group of providers in a multidisciplinary team, the patient can benefit from:4,6,7
- Integrated skills and knowledge from multiple disciplines
- A coordinated and comprehensive treatment plan
Who are the key specialists in the DMD multidisciplinary care team
Neuromuscular management4
KEY ROLE: To optimise the maintenance of muscle strength and function, lead the multidisciplinary clinic and act as first point of contact to families.
A neuromuscular specialist:
- Leads, administers and coordinates the DMD multidisciplinary clinic
- Characterises the patient’s disease trajectory and defines the treatment plan
- Provides patient and family support and education
- Initiates and manages use of pharmaceutical interventions

Rehabilitation management4
KEY ROLE: To provide physical, occupational, and speech and language therapy.
Professionals including physical therapists, occupational therapists, speech-language pathologists, orthotists and medical equipment providers:
- Help prevent or manage muscle/joint contracture, deformity, falls and fractures
- Help prevent or manage pain
- Promote exercise and activity
- Provide orthoses, equipment and learning support
Cardiac management4,6
KEY ROLE: To evaluate cardiac function and manage cardiac complications.
A cardiologist:
- Monitors cardiac function and conducts cardiac assessments (in both DMD patients and female carriers)
- Initiates and manages cardiac pharmacological therapies
- Uses heart failure interventions with deterioration of function
Respiratory management4,6
KEY ROLE: To evaluate respiratory function and manage respiratory complications.
Professionals including physicians and respiratory or physical therapists:
- Monitor respiratory muscle function
- Manage lung volume recruitment, assisted coughing, nocturnally assisted ventilation and subsequent daytime ventilation
- Manage immunisation schedules
Orthopaedic & surgical management4,6
KEY ROLE: To manage joint contractures and scoliosis.
Professionals including physical therapists, occupational therapists, rehabilitation physicians, neurologists, orthopaedic physicians and social workers:
- Provide surgical interventions to manage contractures and scoliosis
- Provide physical therapy before and after surgery
Bone health management4,6
KEY ROLE: To diagnose and treat osteoporosis.
A bone heath expert:
- Identifies early indications of bone fragility
- Initiates and manages intravenous bisphosphonate therapy to treat osteoporosis
Psychosocial management4,7
KEY ROLE: To manage learning, emotional and behavioural disorders.
Professionals including mental health clinicians, occupational therapists and physical therapists:
- Assess mental health and educational needs
- Provide neuropsychological evaluation/interventions for learning, emotional and behavioural problems

Specialist nursing8
KEY ROLE: To provide practical and emotional support for families affected by DMD.
Specialist nurses:
- Provide advice and information to patients and families about DMD
- Support a patient’s physical and emotional wellbeing

Genetic counselling9,10
KEY ROLE: To manage genetic testing and explain what the results mean for families.
A genetic counsellor:
- Provides education about DMD
- Coordinates and explains genetic testing
- Provides emotional counselling
- Discusses family planning options
Gastrointestinal and nutritional management4
KEY ROLE: To promote a healthy diet and weight, and manage any gastrointestinal problems.
A dietitian nutritionist:
- Monitors growth and weight to prevent undernutrition, malnutrition or obesity
- Promotes a healthy, balanced diet
A gastroenterologist:
- Manages constipation, gastroesophageal reflux, gastrointestinal motility concerns and gastrostomy tube placement
Regional care services8,11
KEY ROLE: To provide practical and emotional support for families affected by DMD.
Regional neuromuscular care advisors:
- Help support patients in school and work environment
- Assist in planning for major housing adaptations and equipment resources
- Support the transition from child to adult medical care
- Advise patients on disability benefit assessments
- Educate other healthcare professionals about DMD

Endocrine management4
KEY ROLE: to manage endocrine complications of DMD and initiate hormone replacement therapy.
An endocrinologist:
- Manages hormone deficiencies and hormone replacement therapy in the case of impaired growth or delayed puberty onset
- Educates families on the risks of adrenal crisis following glucocorticoid termination
Three two-page summaries of the 2018 International Duchenne Care Considerations are available in PDF format for download.
Diagnosis and management of Duchenne muscular dystrophy – Part 1
Diagnosis, and neuromuscular, rehabilitation, endocrine, and gastrointestinal and nutritional management.
Diagnosis and management of Duchenne muscular dystrophy – Part 2
Respiratory, cardiac, bone health and orthopaedic management.
Diagnosis and management of Duchenne muscular dystrophy – Part 3
Primary care, emergency management, psychosocial care, and transitions of care across the lifespan.
Physiotherapy exercise book for younger children
Younger children
Download this exercise book to help younger children get the most out of their physiotherapy treatment
Physiotherapy exercise book for older children
Older children
Download this exercise book to help older children get the most out of their physiotherapy treatment
E-book: Postural management and stretches e-book for adults with DMD
Adults
Download this e-book on postural management and stretches, designed for adult patients with DMD
Patient experience: Physiotherapy for DMD
From first recognising symptoms to ongoing support for maintaining mobility, find out the important role physiotherapy plays for Kevin, a young patient with DMD.
Stretching the goals of care: Physiotherapy and improving outcomes in DMD
Helping patients with DMD to maintain mobility and function can help to improve quality of life and outcomes.4 As such, specialist physiotherapy is important in DMD treatment.
Access the Expert Insights page to watch the ‘Stretching the goals of care’ webinar, and find out more about:
- Signs and symptoms of DMD
- Time-function tests and their impact on outcome measurements
- The importance of maintaining mobility in patients with DMD
- The use of passive stretching and physical exercise in DMD to improve patient mobility and function
Pharmacological treatment for DMD
There are different approaches to pharmacological management, including:
Glucocorticoids, a mainstay therapy, for the treatment of muscle strength and function.3,4
Angiotensin-converting enzyme inhibitors or angiotensin receptor blockers for the treatment of heart disease.6
Bisphosphonate therapy for the treatment of osteoporosis.6

Hormone replacement therapy for the treatment of impaired growth, delayed puberty, and adrenal insufficiency.4
Additional therapeutic strategies include:†13

Mutation-specific therapies or gene replacement therapies aiming to restore dystrophin production.

Muscle membrane stabilisation and/or upregulation of compensatory proteins which are structurally and functionally similar to dystrophin

Reduction of the inflammatory cascade and/or enhancement of muscle regeneration.
Along with physiotherapy, treatment with glucocorticoids remains key to DMD treatment and it is recommended that individuals should continue taking glucocorticoids after loss of ambulation.4
Recent studies have also demonstrated the benefits of early glucocorticoid treatment, before significant physical decline.4,15
The long-term effects of glucocorticoid therapy (compared to untreated patients) have been shown to include: 3,4,14,15
Preserved muscle strength and motor function.

Delayed loss of ambulation.
Preserved pulmonary function.
Avoidance of scoliosis surgery.
Improved survival.
The 2018 International Care Guidelines recommend following an initial consultation with the family, a discussion regarding side effects, and a nutritional consultation should occur before any glucocorticoid treatment is initiated.4 Well-documented side effects of long-term corticosteroid use can include; weight gain and obesity, acne and warts, cushingoid features, growth retardation and delayed puberty, cataracts, immune/adrenal suppression, glucose intolerance, hypertension, adverse behavioural changes, gastro-oesophageal reflux, peptic ulcer, gastritis, osteoporosis and myoglobinuria.16
The transition from paediatric to adult care
People with DMD need education and support to make transitions throughout their lifespan.7
Transition planning should begin in early childhood.7
Individuals with DMD should be encouraged to participate fully in future planning of their care.7 They should be assisted in the transition from paediatric healthcare, which is family-centred, to adult healthcare, which is patient-centred and focused on independence.7
A care coordinator or social worker should be responsible for transition planning.7
Components of young adulthood that should be addressed during transition planning include:7
- Healthcare
- Activities of daily living
- Education or employment
- Relationships with others
- Housing
- Transportation
Transition toolkit: Overview for patients
A guide for DMD patients on managing the condition, and making informed health-related choices.
Transition toolkit: Patient medical summary
A handy document for recording patient information, which can be passed from paediatric neurologists to adult neurologists.
Transition toolkit: Transition guide for patients
A guide for young men with DMD on preparing for a successful transition from paediatric to adult care.
Transition toolkit: Overview for adult neurologists
A guide for adult neurologists on how to manage the treatment of young men with DMD.
Transition toolkit: Checklist for adult neurologists
A brochure for adult neurologists on how to help young men with DMD transition from paediatric to adult care.
Transition toolkit: Digital consensus guidelines for the standard of care of adults with DMD
The Adult North Star Network’s consensus guidelines for the standard of care of adults with DMD, in digital format.
Transition toolkit: Print consensus guidelines for the standard of care of adults with DMD
The Adult North Star Network’s consensus guidelines for the standard of care of adults with DMD, in print format.
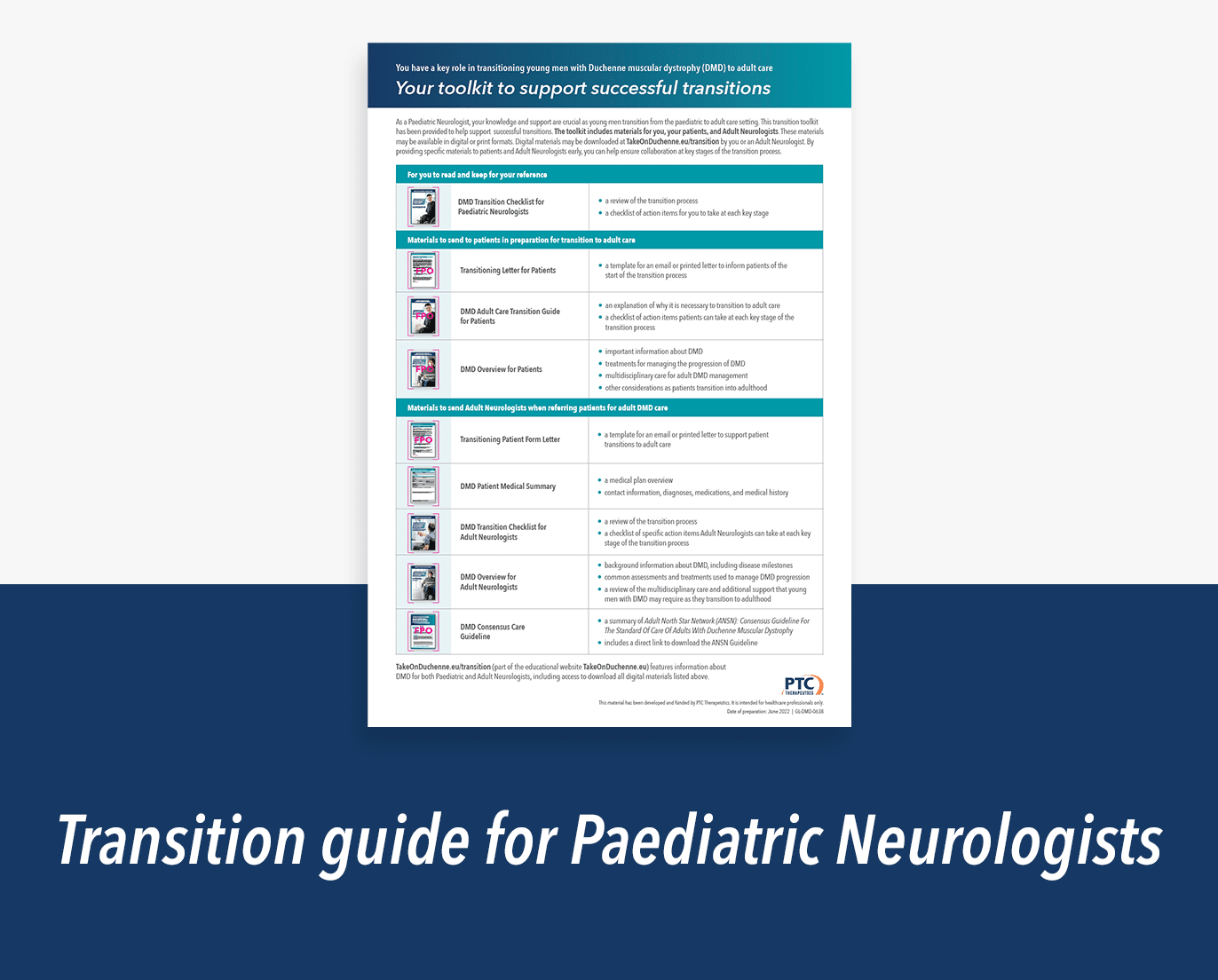
Transition toolkit: Transition guide for paediatric neurologists
A guide for paediatric neurologists on how to support the successful transition of DMD patients from paediatric to adult care.
Transition toolkit: Transition brochure for paediatric neurologists
A brochure for paediatric neurologists explaining how to provide critical support for young men with DMD transitioning to adult care.
Psychological care for DMD
The psychological manifestations of DMD vary widely; some patients may have extensive neurodevelopmental or psychological disorders, while others may not.7
The psychological effects of DMD need to be considered and monitored across all stages of the disease for affected individuals and their families.7
Mental health and quality of life should be screened at each neuromuscular clinic visit, either informally or through standardised assessments. Recommended tests include:7
For children with DMD
- Strengths and Difficulties Questionnaire
For adults with DMD
- Patient Health Questionnaire 9-item depression scale
- Generalized Anxiety Disorder 7-item scale (GAD-7)
For parents of children aged 5–17 years with DMD
- Personal Adjustment and Role Skills Scale (PARSIII)
If screening identifies concerns regarding any aspects of mental health or psychological wellbeing, referrals should be made to psychologists or psychiatrists for further evaluation and potential intervention.7
In instances where formal or pharmacological interventions are required, standard prescribing habits should be followed.7
All individuals and their families with DMD should expect to live rich, fulfilling lives and, therefore, psychological monitoring and care is an important aspect of ensuring this ambition is possible.7
Want to hear more on DMD from leading clinicians? Listen to DMD expert insights on reaching a timely diagnosis and managing DMD.
Learn moreChange your specialty
Thank you for entering your specialty to view this site, if you wish to change your selection, please select an alternative specialty below:


Duchenne muscular dystrophy expert insights
Find out more about DMD, and learn from leading clinicians.


Duchenne muscular dystrophy key publications
Read some of the latest scientific and clinical research on DMD.


E-learning tool for health care professionals
Access to e-Learning modules for healthcare professionals to help you understand your role in identifying and managing Duchenne muscular dystrophy

The content on this page has been reviewed by Dr Christian Werner, Executive Director, Global Medical Affairs
Global Duchenne Muscular Dystrophy Lead, PTC Therapeutics.
This page has been through comprehensive review for informational and educational purposes. Find out more about our content review process.
*Please note that the information in below is intended to provide an overview only and is not exhaustive information. Please refer to the international care guidelines and any local guidelines for more information.
†Some of these treatments have been approved by regulators while others are near, or in, regulatory review or in clinical trials and might become available in the future.4,12
References
- Laing NG et al. Clin Biochem Rev. 2011;32(3):129–134.
- Blake DJ et al. Physiol Rev. 2002;82(2):291–329.
- Bushby K, et al. Lancet Neurol.2010;9:177–189.
- Birnkrant DJ, et al. Lancet Neurol.2018;17:251–267.
- Aartsma-Rus A, et al. J Pediatr. 2019; 204:305–313.e4.
- Birnkrant DJ, et al. Lancet Neurol. 2018:17:347–361.
- Birnkrant DJ, et al. Lancet Neurol. 2018:17:445-455.
- Muscular Dystrophy UK. Care Advisers. Available at: https://www.musculardystrophyuk.org/get-support/support-services-in-your-area/care-advisors [Accessed November 2022].
- Helderman-van den Enden AT. et al. Clin Genet. 2011:79:236–242.
- Institute of Medicine (US) Committee on Assessing Genetic Risks; Andrews LB, et al. edtors. Assessing Genetic Risks: Implications for health and Social Policy. Washington (DC): National Academies Press (US): 1994. 4, Issues in Genetic Counselling Available at: https://www.ncbi.nlm.nih.gov/books/NBK236049/ [Accessed November 2022].
- John Walton Muscular Dystrophy Research Centre. Specialist care advisor. Available at: https://newcastle-muscle.org/clinical/attending-a-clinic/care-advisor/ [Accessed November 2022].
- Duchenne Connect. Genetic Counseling. Available at: https://www.duchenneconnect.org/genetic-counseling.html [Accessed November 2022].
- Mah JK. Neuropsychiatr Dis Treat. 2016;12:1795–1807.
- Gloss D, et al. Neurology. 2016;86:465–472.
- Merlini L, et al. Muscle Nerve. 2012;45:796–802.
- Nascimento Osorio A, et al. Neurologia. 2019;34:469–481.
© 2022 PTC Therapeutics.
GL-DMD-0713 | October 2023