What are neuromuscular disorders?
Types of neuromuscular disorders
Different types of neuromuscular disorders are generally classified depending on the location of involvement.1 Examples of neuromuscular disorders include:1
- Disorders of the muscle (e.g. Duchenne muscular dystrophy [DMD])
- Disorders of the neuromuscular junction (e.g. congenital myasthenic syndrome)
- Disorders of the peripheral nerve (e.g. Charcot-Marie-Tooth disease)
The majority of neuromuscular disorders that present in childhood have a genetic basis.1
Learn more about DMD inheritance and causes
Neuromuscular disorders symptoms
Children with neuromuscular disorders experience progressive muscle deterioration and an ongoing decline in physical function.2 The earliest and most common sign of neuromuscular disease is muscle weakness, which manifests as delayed motor development.3,4 Delays in language, speech and cognition should also prompt suspicion that something may be wrong.3,5—7
Learn more about DMD symptoms
Why early diagnosis matters
Although these diseases are not curable, treatment and management options for neuromuscular disorders are available.8,9
An early diagnosis can facilitate access to the right treatment and services, which may help improve outcomes and help to avoid life-threatening complications.3,4,8
Learn more about DMD diagnosis
What is muscular dystrophy?
Muscular dystrophies are a group of neuromuscular disorders characterised by progressive muscle degeneration and weakness.2 They are caused by mutations in genes that produce either dysfunctional, or insufficient levels of, proteins that are essential for muscle cell stability.2 Children with muscular dystrophy experience progressive muscle deterioration and an ongoing decline in physical function.2
Muscular dystrophies differ in age of onset, severity, pattern of inheritance, and the muscle groups and other organs affected.2
There are different forms of muscular dystrophy, some of the common types include:2
DMD10,11
DMD is the most common and severe form of muscular dystrophy among children, and accounts for >50% of all cases. It primarily affects males.
Becker muscular dystrophy (BMD)10,11
BMD is less common and severe than DMD, but presents with similar symptoms.
Myotonic muscular dystrophy10
Myotonic is the most common adult form of muscular dystrophy.
Facioscapulohumeral (FSHD) muscular dystrophy10
FSHD refers to the areas affected – the face (facio), shoulders (scapulo) and upper arms (humeral). It typically affects adolescents.
Limb girdle muscular dystrophy10
Most often appears in adolescence or young adulthood. Affects both males and females.
E-learning for healthcare professionals
Interested in learning more on neuromuscular disorders?
Read below to access an e-learning module developed by the Royal College of Paediatrics and Child Health (RCPCH) in the UK.
Recognising neuromuscular disorders — A practical approach
Children with neuromuscular disease experience progressive muscle deterioration and a continual decline in physical function.8 Signs and symptoms usually begin in early infancy, but it can take a long time before a child is diagnosed.3,8 This means missing out on early treatments and interventions that can significantly improve these young patients’ futures.
This e-learning module will help you recognise the early signs of muscle disease so you can refer your patients with confidence.
- Developed by experts at Newcastle Muscle Centre and Newcastle University in collaboration with the RCPCH
- Free to take
- Only takes 1 hour to complete
- CME-accredited in the UK
This e-learning module has been supported by a financial grant from PTC Therapeutics. PTC Therapeutics have had no involvement in the development of the content of this module.
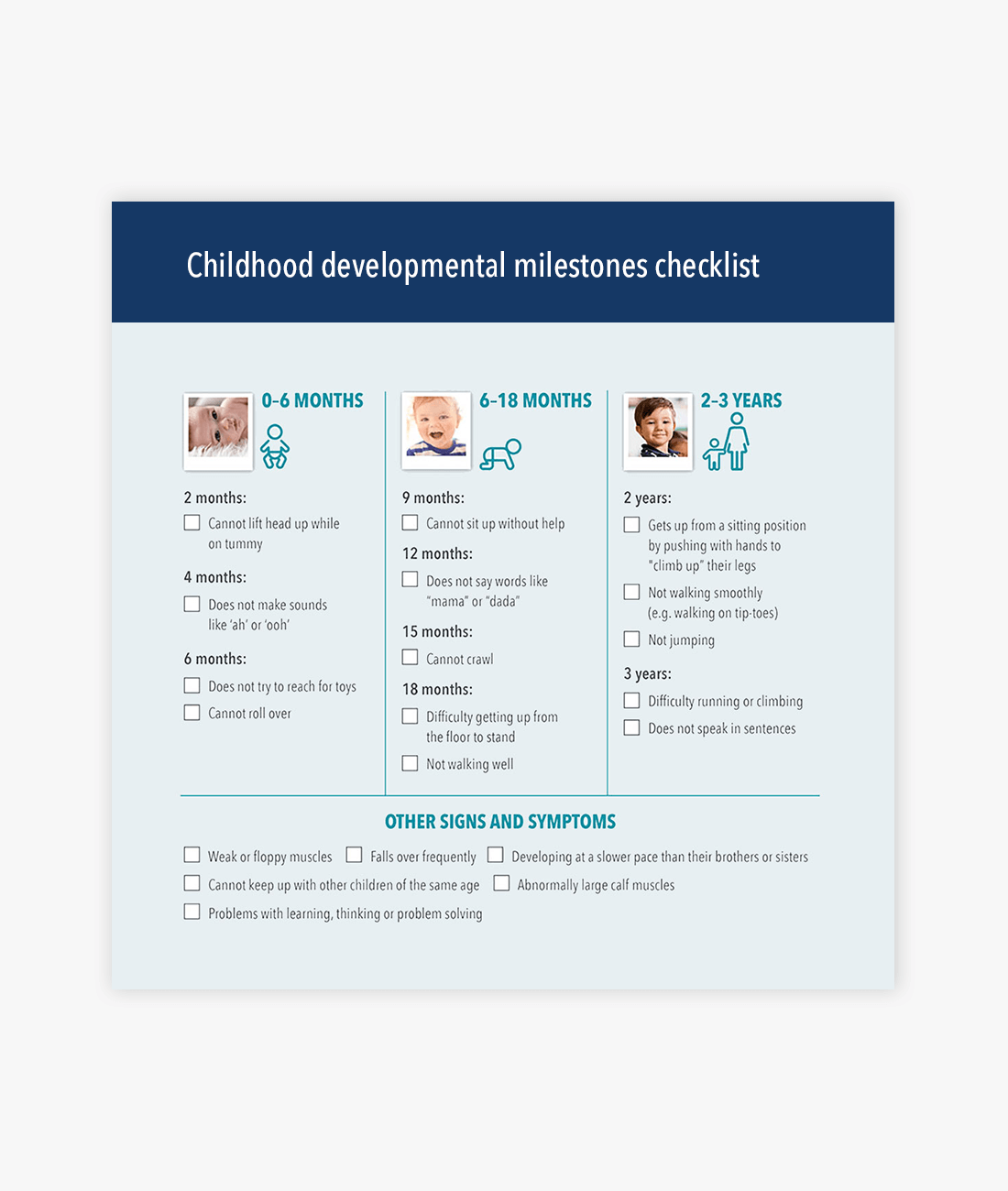
Download the developmental milestones checklist
Use the developmental milestones checklist to help identify warning signs for developmental delays in children from birth to 3 years of age.
What exactly is Duchenne muscular dystrophy? Find out more below
Learn More

What is Duchenne muscular dystrophy?
DMD is a rare genetic neuromuscular disorder that causes progressive muscle damage and degeneration8


Duchenne muscular dystrophy causes and inheritance
DMD is a hereditary X-linked recessive neuromuscular disorder caused by mutations in the dystrophin gene8


Duchenne muscular dystrophy symptoms
Early childhood signs and symptoms of DMD include weakness, clumsiness, Gowers’ sign, difficulties with stair-climbing or toe walking8


Duchenne muscular dystrophy diagnosis
An early and accurate diagnosis of DMD is a crucial aspect of care8

The content on this page has been reviewed by Dr Christian Werner, Executive Director, Global Medical Affairs
Global Duchenne Muscular Dystrophy Lead, PTC Therapeutics.
This page has been through comprehensive review for informational and educational purposes. Find out more about our content review process.
References
- Dowling JJ, et al. Am J Med Genet A. 2018;176:804–841.
- Theadom A, et al. Neuroepidemiology. 2014;43:259–268.
- van Ruiten HJ, et al. Arch Dis Child. 2014;99:1074–1077.
- Lurio JG, et al. Am Fam Physician. 2015;91:38–44.
- Noritz GH, et al. Pediatrics. 2013;131:e2016–e2027.
- Miller N, et al. S Afr J Commun Disord. 2012;59:27–33.
- Cyrulnik SE, et al. J Pediatr. 2007;150:474–478.
- Birnkrant DJ, et al. Lancet Neurol. 2018;17(3):251–267 [Part 1].
- National Task Force for Early Identification of Childhood Neuromuscular Disorders. Child Muscle Weakness. 2022. Available at: www.childmuscleweakness.org [Accessed November 2022].
- National Institutes of Health. What are the types of muscular dystrophy? 2020. Available at: https://www.nichd.nih.gov/health/topics/
musculardys/conditioninfo/types [Accessed November 2022]. - Andrews JG, et al. Adolesc Health Med Ther. 2018;9:53–63
© 2022 PTC Therapeutics.
GL-DMD-0707 | October 2023