The importance of early DMD diagnosis
An early and accurate DMD diagnosis is important.1–3
- Early and accurate diagnosis of DMD is critical because once muscle function is lost, it cannot be restored4–7
- Timely and accurate diagnosis can enable the patient and family to receive the care and support they need7–9
- Early and accurate diagnosis ensures early access to treatment, counselling and appropriate screening for possible complications8
- Early treatment may give improved long-term patient outcomes8
Healthcare professionals play a key role in recognising the red flag signs and symptoms of DMD.7
- DMD usually presents between 2 and 5 years of age, but signs of weakness may be evident earlier3–5
- Gowers’ manoeuvre, characterised by an inability to rise from the floor without pulling or pushing up with the arms, is a classic symptom of DMD1,10–12
- However, this symptom would not trigger concerns until the child is 2–3 years of age13
- There are earlier key motor and non-motor developmental milestones that may be missed in a child presenting with a neuromuscular disorder and children with DMD, for example, difficulty rising to stand and not walking well by 16–18 months7,11,12,14
What is a creatine kinase (CK) test?
CK is an enzyme found in skeletal muscle as well as in the heart, brain and other tissues. Increased amounts of CK are released into the blood when there is muscle damage.12 Elevated CK levels reflect muscle damage in patients with DMD, making it an important diagnostic marker for the condition.8
Children with developmental delays should have a CK test as it could be due to a neuromuscular disorder.7,8,11
When to order a CK test
A CK test should be carried out if:
- Examination and medical history suggest progressive muscle weakness11,12,15
- A child has delayed motor function, such as not walking well or not able to rise to stand by 18 months7,11,12,16
- A child shows developmental delay, including delays with mixed presentation (e.g. speech and cognition), and evaluation suggests a peripheral neuromuscular problem11
- A child has a positive family history of DMD and suspicion of abnormal muscle function7
- Blood tests reveal an unexplained increase in transaminases7
What the results mean:7,12
If CK is elevated
The normal range is generally up to 250 U/L*.12 If CK levels are above this, refer the patient to neuromuscular specialist for DMD gene testing.7
If CK is normal
This does not rule out other neuromuscular disorders.12
All patients who have elevated CK levels should be promptly referred to a neuromuscular specialist.2,10
Normal or mildly elevated CK does not rule out a neuromuscular disorder. If a patient has missed motor milestones, they should also be referred to a neuromuscular specialist.2
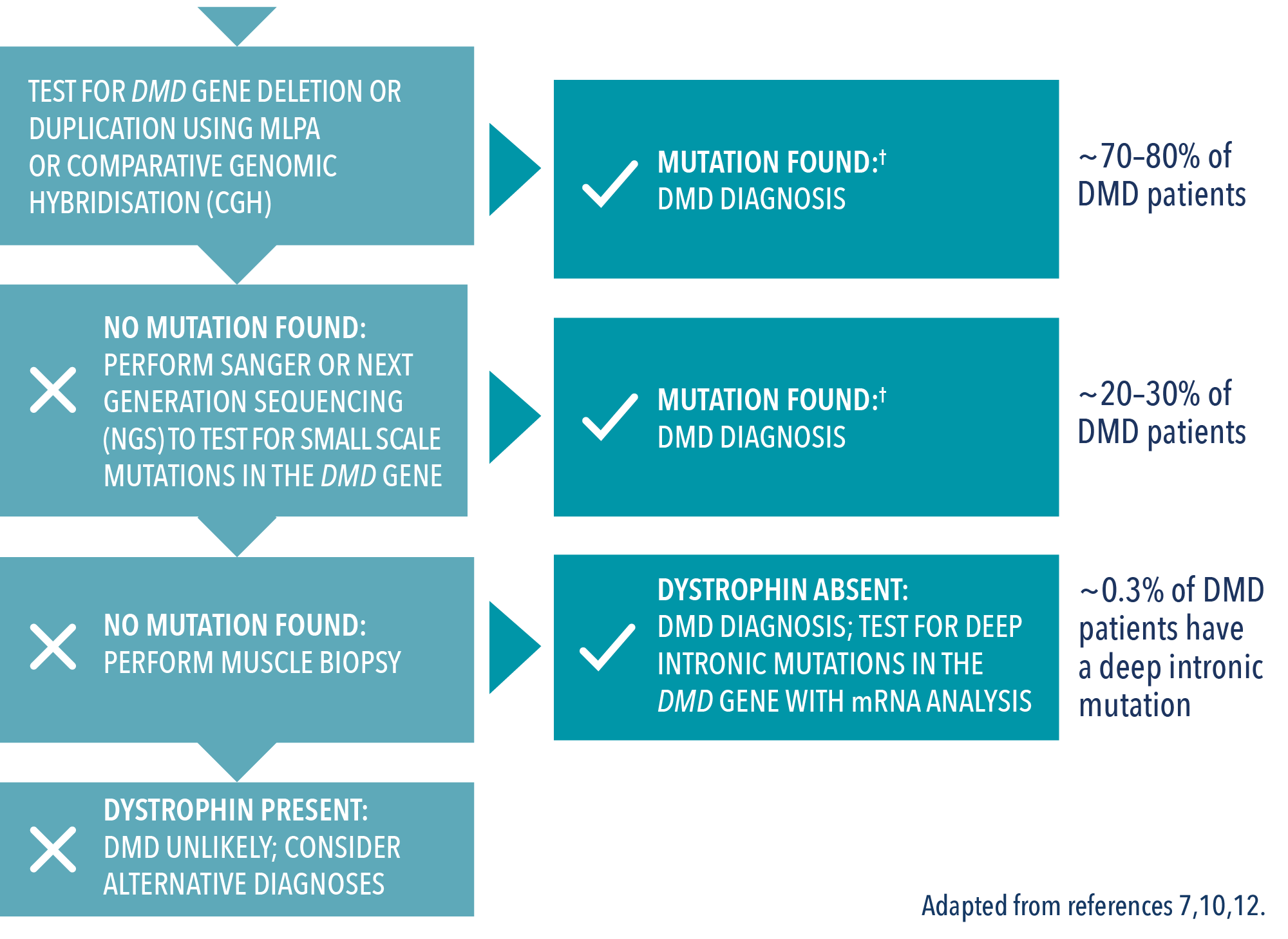
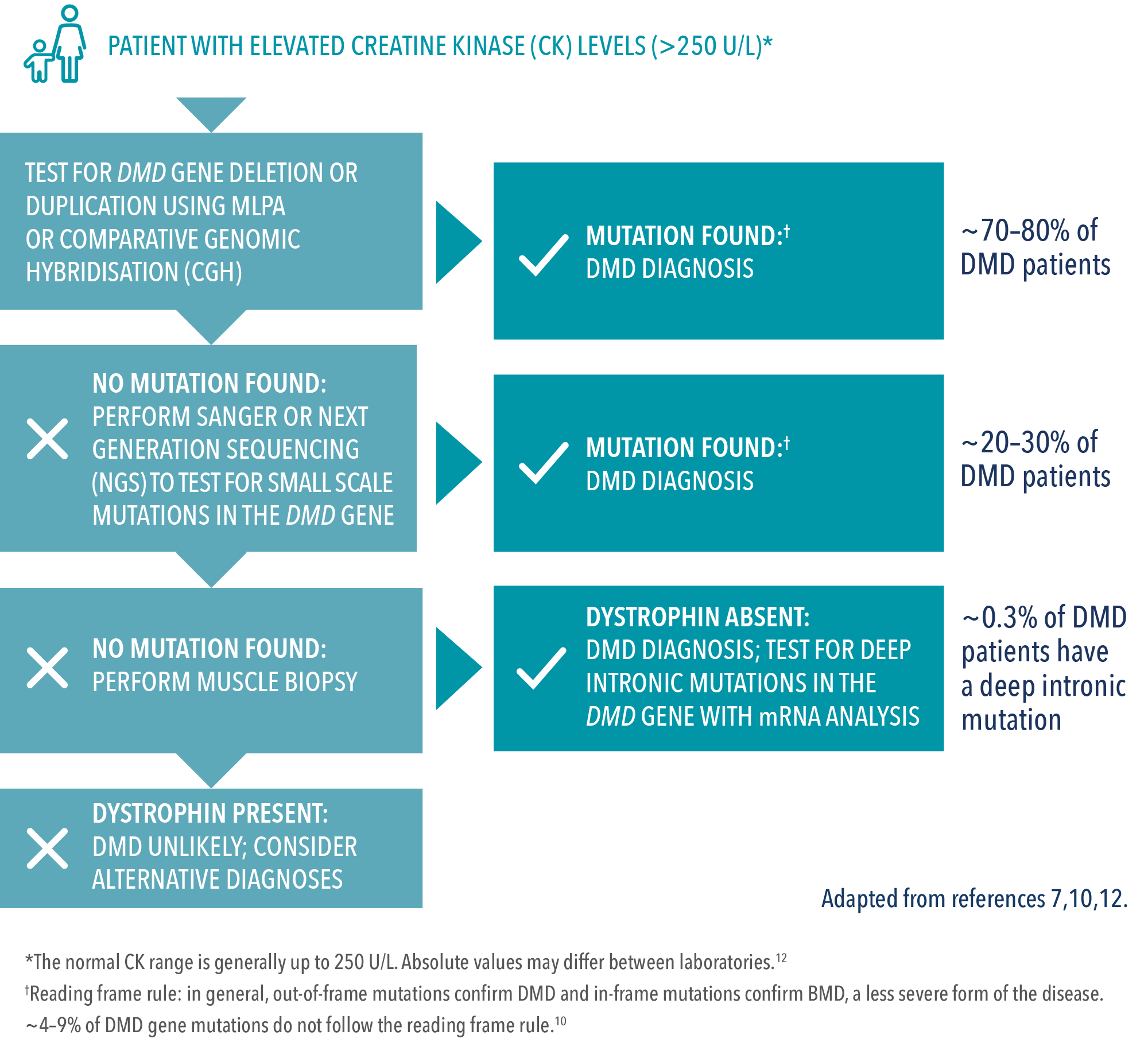
Genetic testing for DMD
Genetic testing is the only method for determining a patient’s specific mutation type.7,10 This is important because a specific genetic diagnosis may help identify medical management options and the potential to enrol in clinical trials.10
Additionally, once a mutation is identified, female relatives can find out their carrier status. This is important for two main reasons:10
- Female carriers can pass DMD on to their children
- Female carriers need medical assessment and follow-up
A genetic diagnosis involves two types of tests:
First-level testing7,17
- The majority of mutations (~70%) are detected by multiplex ligation-dependent probe amplification (MLPA)
- MLPA can detect both large deletions and large duplications in patients and carriers
Second-level testing:7
- If no mutation is found, gene sequencing should be performed
- Only gene sequencing can definitely detect smaller mutation types. These mutations include point mutations (nonsense or missense), small deletions, and small duplications or insertions
Interested in reading real-life stories about the DMD diagnosis process?
Find out more at the link below
Case study stories about diagnosing Duchenne Access expert insights: Diagnosing DMD
The implications of DMD diagnosis
One diagnosis of DMD can impact an entire family. Genetic counselling can help patients and relatives to manage the implications of DMD diagnosis.23–25
Find out more about the benefits of Genetic counselling.
Patient experience: Receiving a diagnosis
Hear how genetic testing played an important role in reaching a DMD diagnosis for Kevin and his family.
Change your speciality
Thank you for entering your specialty to view this site, if you wish to change your selection, please select an alternative specialty below:


Genetic counselling
Genetic counselling offers many benefits for families diagnosed and living with DMD23–25


Duchenne muscular dystrophy treatment
The best outcomes for DMD patients are likely to result from the early application of DMD treatments10,26,2


Duchenne muscular dystrophy expert insights
Find out more about DMD, and learn from leading clinicians, in our Expert Insights section


Duchenne muscular dystrophy key publications
Read some of the latest scientific and clinical research on DMD

The content on this page has been reviewed by Dr Christian Werner, Executive Director, Global Medical Affairs
Global Duchenne Muscular Dystrophy Lead, PTC Therapeutics.
This page has been through comprehensive review for informational and educational purposes. Find out more about our content review process.
References
- Noritz GH, et al. Pediatrics. 2013;131:e2016–e2027.
- National Task Force for Early Identification of Childhood Neuromuscular Disorders. Child Muscle Weakness. 2019. Available at: https://childmuscleweakness.org [Accessed November 2022].
- Ciafaloni E, et al. J Pediatr. 2009;155:380–385.
- Humbertclaude V, et al. Eur J Paediatr Neurol. 2012;16:149–160.
- Blake DJ, et al. Physiol Rev. 2002;82:291–329.
- Laing NG, et al. Clin Biochem Rev. 2011;32:129–134.
- Birnkrant DJ, et al. Lancet Neurol. 2018;17:251–267.
- van Ruiten HJ, et al. Arch Dis Child. 2014;99:1074–1077.
- McDonald CM, Fowler WM. Phys Med Rehabil Clin N Am. 2012;23:475–493.
- Aartsma-Rus A, et al. J Pediatr. 2019;2014:305–313.e14.
- Lurio JG, et al. Am Fam Physician. 2015;91:38–44.
- National Task Force for Early Identification of Childhood Neuromuscular Disorders. Guide for primary care providers. Available at: https://childmuscleweakness.org/wp-content/uploads/2019/05/PrimaryCareProviderPacket.pdf [Accessed November 2022].
- Parsons EP, et al. Eur J Paediatr Neurol. 2004;8:145–153.
- Centers for Disease Control and Prevention. Developmental milestones. Available at: https://www.cdc.gov/ncbddd/actearly/pdf/checklists/all_checklists.pdf [Accessed November 2022].
- Chakrabarty T, et al. Arch Dis Child Educ Pract Ed. 2020;105(3):157–163.
- WHO Multicentre Growth Reference Study Group. Acta Paediatr. 2006;450:86–95.
- Verma PK, et al. Indian J Hum Genet. 2012;18:91–94.
- Bushby K, et al. Lancet Neurol. 2010;9(1):77–93.
- Apkon SD, et al. Pediatrics. 2018;142(Suppl 2):S82–S89.
- Wright MA, et al. J Am Board Fam Med. 2012;25(4):536–40.
- Aartsma-Rus A et al. J Med Genet. 2016;53:145–51.
- Birnkrant DJ, et al. Lancet Neurol. 2018;17(5):445–455.
- Helderman-van den Enden AT, et al. Clin Genet. 2011;79:236–242.
- Institute of Medicine (US) Committee on Assessing Genetic Risks; Andrews LB, et al. editors. Assessing Genetic Risks: Implications for Health and Social Policy. Washington (DC): National Academies Press (US); 1994. 4, Issues in Genetic Counseling. Available at: https://www.ncbi.nlm.nih.gov/books/NBK236049/ [Accessed November 2022].
- Duchenne Connect. Genetic Counseling. Available at: https://www.duchenneconnect.org/genetic-counseling.html [Accessed November 2022].
© 2022 PTC Therapeutics.
GL-DMD-0711 | October 2023