What is DMD?
DMD is the most common and severe form of muscular dystrophy among children and accounts for over 50% of all cases.3
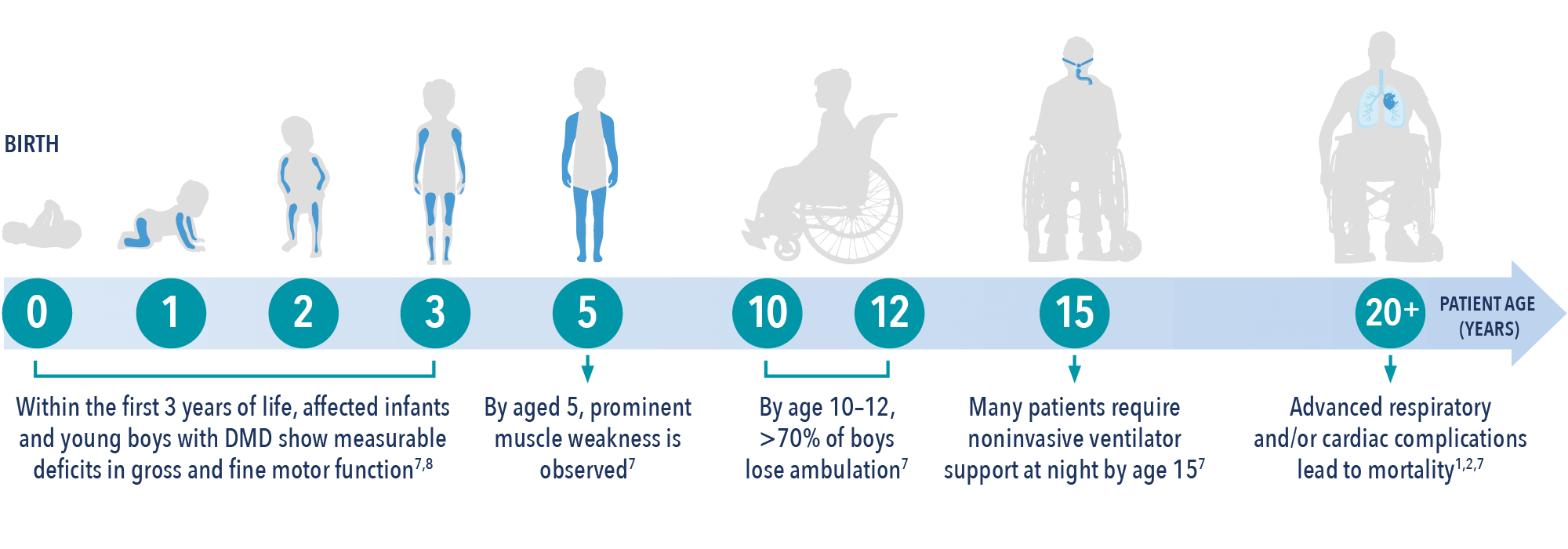
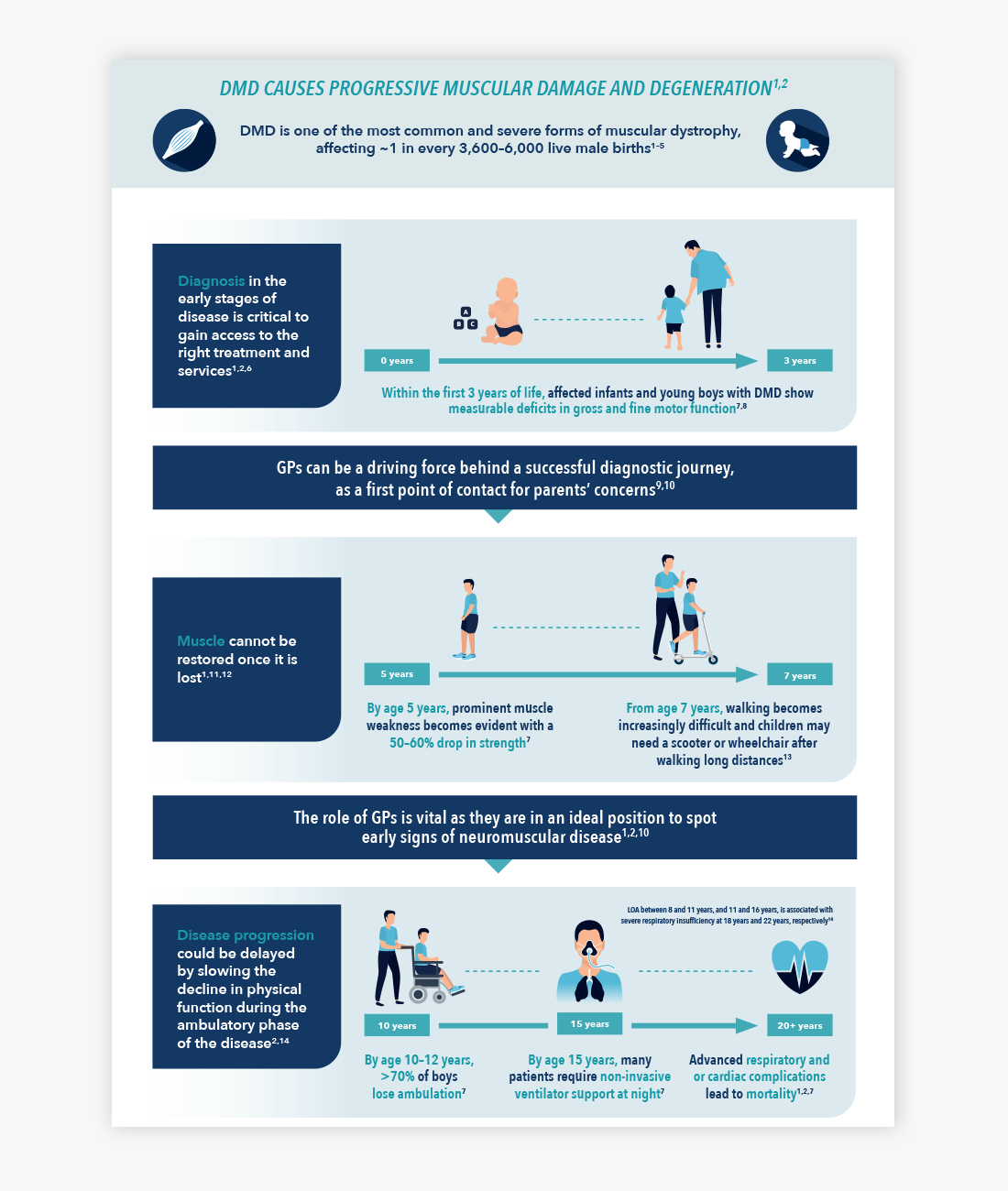
Caused by a mutation in the dystrophin gene, which leads to the absence of, or defects in, dystrophin (an essential protein in the muscle cell membrane), DMD is characterised by progressive decline in muscle function, leading to loss of ambulation and respiratory and cardiac failure.1,2,4
- Children with DMD suffer with progressive muscle deterioration and an ongoing decline in physical function5
- Muscle weakness becomes apparent in early childhood, and, on average, patients require a wheelchair by the early teenage years3,5,6
- Ultimately, progressive muscle degeneration causes respiratory and cardiac failure, leading to early death1
Early intervention may improve patient outcomes1,2
- Once muscle is lost, it cannot be restored9,10
- Early diagnosis is critical to gain access to the right treatments and services1,2,11
- The role of primary care is vital as they are in an ideal position to spot early signs of neuromuscular disease, and therefore make a timely referral2,11,12
Timely and accurate diagnosis can enable the patient and their family to receive the care and support they need.1,2,13
Learn more about DMD diagnosis
How common is DMD?
DMD is one of the most common and severe forms of muscular dystrophy, affecting ~1 in every 3,500—5,000 live male births worldwide.1–4
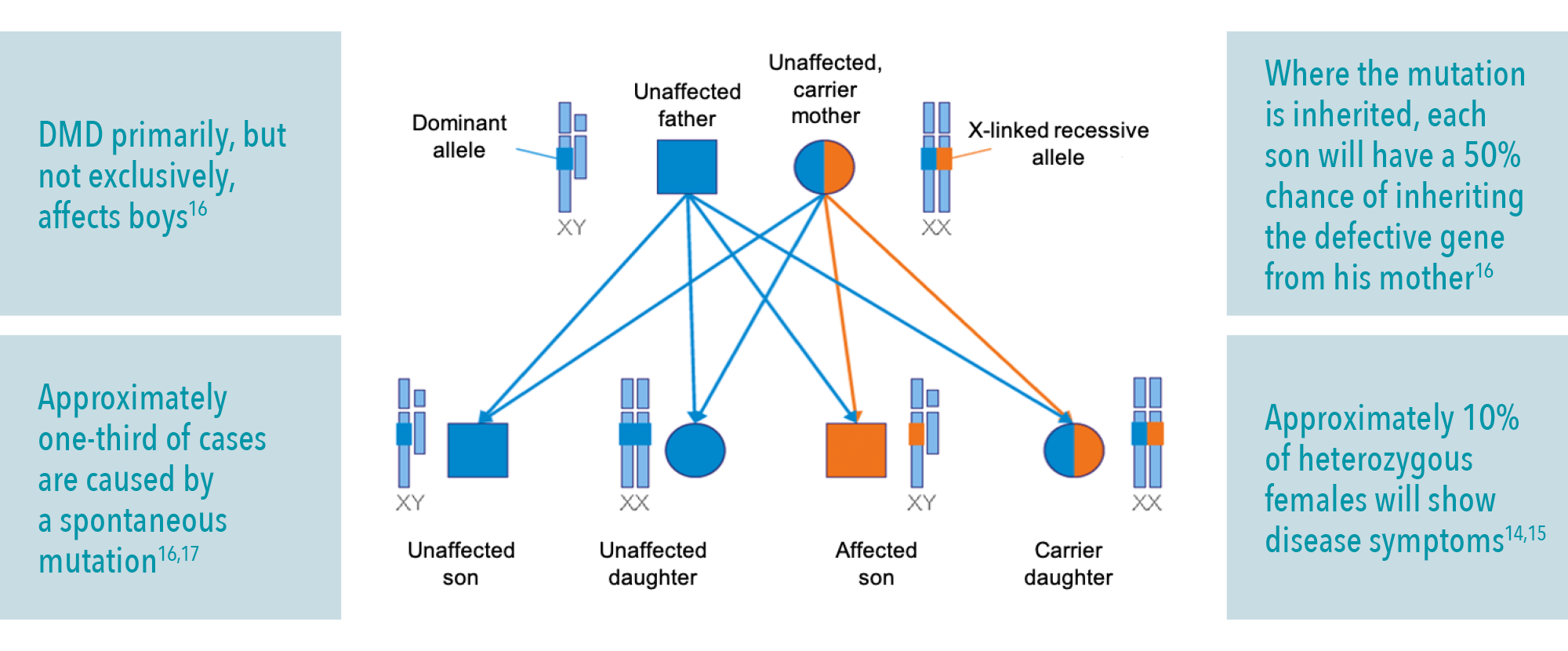
What type of genetic disorder is DMD?
DMD is an x-linked recessive disorder and, as such, it primarily affects males.1,14
If a female carries the mutation in the dystrophin gene (on one of the two X-chromosomes) she may also be affected by DMD; approximately 10% of female carriers show some disease manifestations, with cardiac involvement a frequent finding.14,15
Learn more about DMD symptoms.
Download the infographic: How DMD causes progressive muscular degeneration
Download this handy infographic to find out how DMD causes progressive muscular degeneration throughout a lifespan


Duchenne muscular dystrophy causes and inheritance
DMD is a hereditary X-linked recessive neuromuscular disorder caused by mutations in the dystrophin gene1


Duchenne muscular dystrophy symptoms
Early childhood signs and symptoms of DMD include weakness, clumsiness, Gowers’ sign, difficulties with stair-climbing or toe walking1


Duchenne muscular dystrophy diagnosis
An early and accurate diagnosis of DMD is a crucial aspect of care1


Genetic counselling
Genetic counselling offers many benefits for families diagnosed and living with DMD19—21

The content on this page has been reviewed by Dr Christian Werner, Executive Director, Global Medical Affairs
Global Duchenne Muscular Dystrophy Lead, PTC Therapeutics.
This page has been through comprehensive review for informational and educational purposes. Find out more about our content review process.
References
- Birnkrant DJ, et al. Lancet Neurol. 2018;17:251–267.
- van Ruiten HJ, et al. Arch Dis Child. 2014;99:1074–1077.
- National Institutes of Health. What are the types of muscular dystrophy? Available at: https://www.nichd.nih.gov/health/topics/musculardys/conditioninfo/types [Accessed November 2022].
- Ellis JA, et al. Neuromuscul Disord. 2013;23:682–689.
- Theadom A, et al. Neuroepidemiology. 2014;43:259–268.
- Ciafaloni E, et al. J Pediatr. 2009;155:380–385.
- Mendell JR, Lloyd-Puryear M. Muscle Nerve. 2013;48:21–26.
- van Dommelen P, et al. Dev Med Child Neurol. 2020; doi: 10.1111/dmcn.14623.
- Blake DJ, et al. Physiol Rev. 2002;82:291–329.
- Laing NG, et al. Clin Biochem Rev. 2011;32:129–134.
- Noritz GH, et al. Pediatrics. 2013;131:e2016–e2027.
- Birnkrant DJ, et al. Lancet Neurol. 2018;17:445–455.
- McDonald CM, Fowler WM. Phys Med Rehabil Clin N Am. 2012;23:475–493.
- Bushby K. et al. Lancet Neurol. 2010;77–93.
- Florian A, et al. Eur Heart J Cardiovasc Imaging. 2016;17:326–333.
- MDA. DMD muscular dystrophy (DMD): causes/inheritance. Available at: https://www.mda.org/disease/duchenne-muscular-dystrophy/causes-inheritance [Accessed November 2022].
- Ciafaloni E, et al. J Pediatr. 2009;155:380–385.
- Dent KM, et al. Am J Med Genet. 2005;134:295–298.
- Helderman-van den Enden AT, et al. Clin Genet. 2011;79:236–242.
- Institute of Medicine (US) Committee on Assessing Genetic Risks; Andrews LB, et al. editors. Assessing Genetic Risks: Implications for Health and Social Policy. Washington (DC): National Academies Press (US); 1994. 4, Issues in Genetic Counseling. Available at: https://www.ncbi.nlm.nih.gov/books/NBK236049/ [Accessed November 2022].
- Duchenne Connect. Genetic Counseling. Available at: https://www.duchenneconnect.org/genetic-counseling.html [Accessed November 2022].
© 2022 PTC Therapeutics.
GL-DMD-0708 | October 2023